Caring for a loved one with a serious illness can be emotionally overwhelming and physically demanding. Caregivers often face a delicate balance between managing their loved one’s symptoms, addressing emotional needs, and coordinating medical care, all while navigating their feelings of stress and exhaustion. In such challenging times, it’s crucial to understand the types of care available, specifically hospice and palliative care. Knowing the differences between these options can help caregivers make informed decisions about the best path forward, ensuring that their loved ones receive the proper care at the right time. This blog aims to clarify the distinctions between hospice and palliative care, offering caregivers a clear understanding of each approach. By understanding the critical aspects of these care options, caregivers can feel more empowered and confident in choosing the most appropriate support for their loved ones during challenging moments.
What is Hospice Care?
Hospice care is a specialized form of healthcare designed for patients who are nearing the end of life. The primary goal of hospice is to provide comfort and enhance the quality of life rather than focusing on curative treatments. This form of care is intended for individuals whose illness has progressed to the point where recovery is no longer expected, and medical interventions are aimed at relieving pain and symptoms rather than trying to cure the illness. Hospice care is holistic, addressing not only the physical needs of the patient but also their emotional, psychological, and spiritual well-being.
Eligibility for hospice care is typically considered when a physician determines that a patient has a life expectancy of six months or less without interventions, based on the progression of their illness. However, hospice care services will extend beyond six months if the patient still qualifies to receive services (qualification is based on a regular evaluation of the patient’s condition). The goal will always remain to ensure their comfort and dignity throughout the end-of-life process. Something important to know is that hospice is 100% covered by Medicare. This means there will be no copayment amount for you out of pocket when you have Medicare Part A.
Hospice services encompass a wide range of support for both the patient and their family. These services include pain and symptom management, emotional support, spiritual guidance, and counseling for both the patient and their loved ones. Additionally, hospice teams offer respite care for caregivers, as well as bereavement counseling to help families cope with the loss of their loved one.
Despite its many benefits, hospice care is often misunderstood. A common misconception is that choosing hospice means “giving up” or that it is only for cancer patients. In reality, hospice care is available to individuals with a wide range of terminal illnesses, including heart disease, lung disease, Alzheimer’s, and other chronic conditions. Hospice does not hasten death but instead provides compassionate care focused on comfort and quality of life during the final stages of an illness.

What is Palliative Care?
Palliative care is a specialized approach to medical care that focuses on relieving symptoms and improving the quality of life for patients with serious, chronic, or life-limiting illnesses. Unlike hospice care, palliative care is not limited to end-of-life situations; it can be provided at any stage of illness and can be offered alongside curative treatments. The primary goal of palliative care is to address the physical, emotional, and psychological challenges that come with managing serious illnesses, while supporting the patient and their family.
Anyone with a serious illness can receive palliative care, regardless of their prognosis or the stage of their disease. It is commonly offered to patients dealing with illnesses such as cancer, heart failure, COPD, kidney disease, dementia, and other long-term conditions. Palliative care can be introduced at any point, from the initial diagnosis through ongoing treatment and recovery or even during hospice care if the illness progresses. When it comes to insurance, Palliative care is covered under Medicare Part B, while hospice is covered under Medicare Part A.
Services offered in palliative care include pain and symptom management, emotional and psychological support, coordination of care between different healthcare providers, and assistance with complex decision-making regarding treatment options. At Wings of Hope, our care team typically consists of providers (doctors/nurse practitioners), licensed medical social workers, chaplains, and volunteers who work together to address each patient’s and their family’s unique needs. Our palliative care also supports family members by offering education, community resources, medication reconciliation, coordination with specialty providers, and reconciliation of medication, coordination with specialty providers, collaboration with existing primary care providers, DME, and medical supplies, depending on the payer source.
Additionally, palliative care patients with chronic conditions will also qualify for our CCM program, providing additional care coverage.
A common misconception about palliative care is that it is only for terminally ill patients or those who are at the end of their lives. In reality, palliative care can benefit patients at any stage of a serious illness and is often used to improve the quality of life during ongoing treatments. It provides relief from symptoms such as pain, shortness of breath, fatigue, and depression, helping patients maintain their dignity and comfort while receiving medical care. Palliative care also helps families navigate the journey of illness with community partners and resources. With Wings of Hope, you are not alone. We will help guide you through this process.
Key Differences Between Hospice and Palliative Care
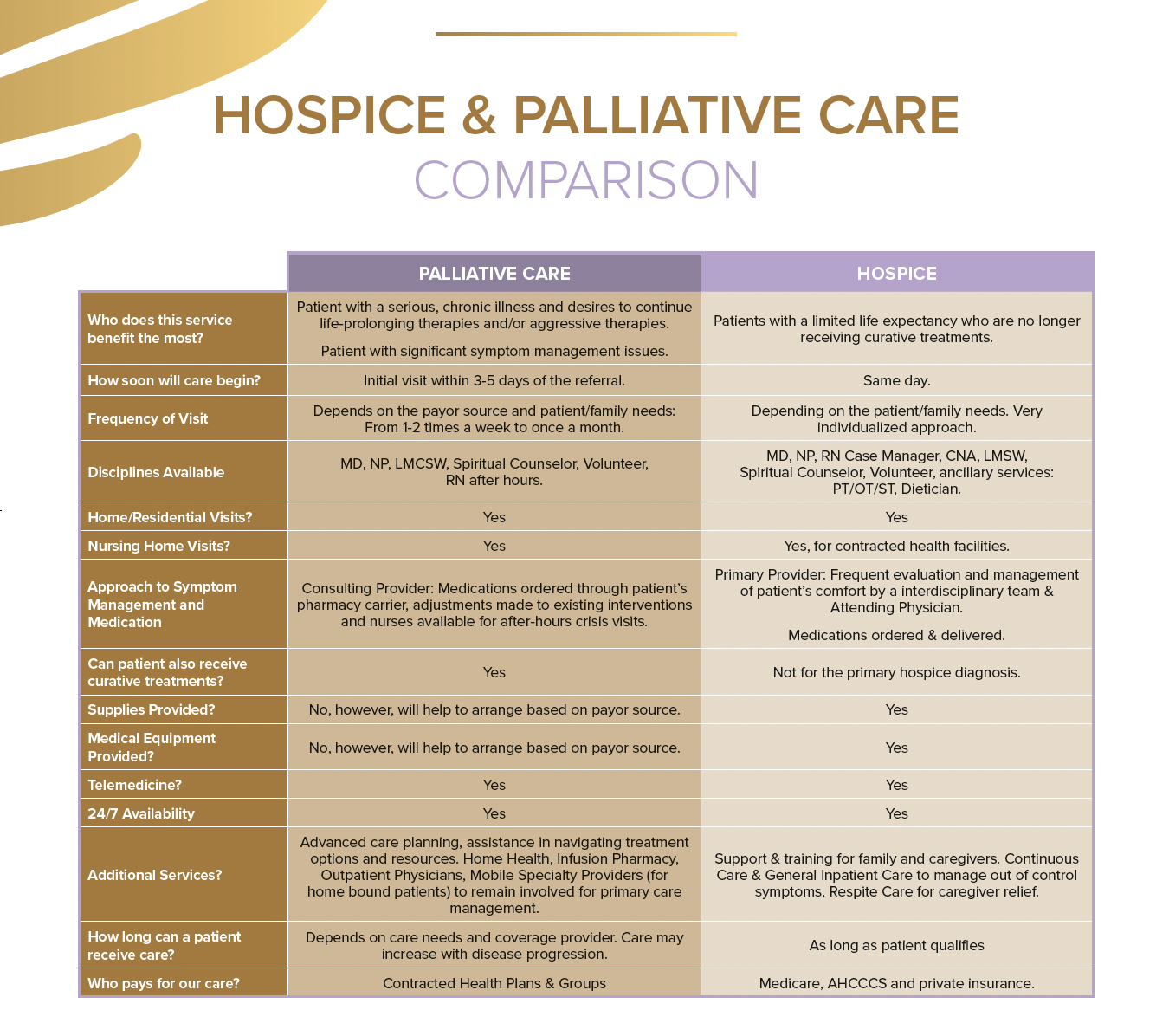
The timing of hospice and palliative care is one of the key distinctions between the two. Palliative care can be initiated at any stage of a serious illness, starting from diagnosis, and can be provided alongside curative treatments. It is designed to offer relief from symptoms and improve the patient’s quality of life while still pursuing treatments to cure or control the illness. On the other hand, hospice care typically begins when curative treatments are no longer pursued, usually when a physician determines that the patient has six months or less to live, without intervention. Hospice care focuses solely on comfort, helping patients live their remaining time with peace and dignity.
The treatment focus also differs significantly between the two. Hospice care is entirely centered on comfort at the end of life, with an emphasis on managing pain and other symptoms rather than seeking to cure the illness. Its goal is to make the patient as comfortable as possible while also providing emotional and spiritual support during the final phase of life. In contrast, palliative care takes a broader approach, providing symptom relief and improving the quality of life at any stage of illness, whether or not the patient is receiving curative treatments. This means palliative care can benefit individuals dealing with long-term conditions who are not necessarily near the end of life.
The goals of each type of care further illustrate these differences. Hospice care ensures that patients spend their final days with dignity, peace, and minimal discomfort. It focuses on the quality of life during the last phase of an illness, supporting both the patient and their family emotionally and spiritually. On the other hand, palliative care aims to enhance the patient’s overall well-being throughout their illness, addressing both physical symptoms and emotional challenges to help them live as comfortably and thoroughly as possible, regardless of their prognosis.
Both hospice and palliative care rely on a multidisciplinary team of professionals to address the patient’s various needs. In hospice care, the team typically includes doctors, nurses, social workers, certified nursing assistants (CNA’s) chaplains, and counselors, all working together to provide holistic end-of-life support. In palliative care, the team is similar and includes doctors, nurses, social workers, and chaplains, but the focus may be more on symptom management and navigating complex medical decisions. Both teams offer comprehensive care, ensuring that the patient’s physical, emotional, and spiritual needs are met. Still, the ultimate goals and timing of care differ depending on whether the patient is receiving palliative or hospice care.
When Should Caregivers Consider Hospice Care?
Hospice care may be appropriate when a loved one shows signs of rapid health decline, such as significant weight loss, frequent infections, or increased weakness and fatigue. Additionally, frequent hospitalizations, emergency room visits, or uncontrolled symptoms like pain, nausea, or breathing difficulties may indicate that hospice care should be considered. Hospice is often introduced when curative treatments are no longer effective, and the focus shifts to ensuring comfort and quality of life.
For caregivers, the decision to transition a loved one to hospice care can be emotionally challenging. It may bring feelings of guilt, sadness, or fear, as it often signals that the end of life is near. Caregivers may struggle with accepting this reality while wanting to provide the best possible care and comfort. It’s important for caregivers to seek emotional support during this time, whether through counseling or support groups.
To initiate hospice care, begin by discussing the option with the patient’s doctor, who can assess whether hospice is the right next step. It’s also important to involve family members in this discussion to ensure everyone understands the goals of hospice care.
Please know, we are only a phone call away to come to you and provide a complimentary assessment to determine whether you qualify for hospice service. We can be reached 24 hours a day at (602) 971-0304. Together, caregivers and healthcare professionals can navigate this decision with compassion, providing the best care for the patient’s final phase of life.
When Should Caregivers Consider Palliative Care?
Palliative care may be appropriate when a loved one is dealing with a serious illness, such as cancer, heart disease, or dementia, and requires ongoing management of symptoms like chronic pain, fatigue, or breathing difficulties. It is particularly beneficial for patients experiencing physical or emotional distress that affects their quality of life, even if they are still receiving curative treatments. Palliative care can be introduced at any stage of illness to help manage symptoms and improve overall well-being.
Palliative care provides significant support for caregivers by offering counseling, education, and being able to provide effective symptom management. It helps caregivers understand how to manage their loved one’s symptoms effectively while also addressing the emotional toll that caregiving can take.
To initiate palliative care, caregivers should begin by openly conversing with their loved one’s healthcare provider. Discuss the current symptoms and quality of life concerns, and ask about options for palliative care. Many hospitals and clinics have palliative care teams, and the doctor can help coordinate a referral. By starting the conversation early, caregivers can ensure their loved one receives comprehensive support tailored to their needs.
The Role of Caregivers in Hospice and Palliative Care
Supporting a loved one in hospice care involves providing emotional support and helping ensure their comfort. Caregivers are crucial in working closely with hospice staff, communicating their loved one’s needs, and participating in care decisions. Hospice care focuses on managing pain and other symptoms, and caregivers help by creating a peaceful environment, offering reassurance, and simply being present during this time. Additionally, caregivers collaborate with hospice professionals to address the patient’s emotional and spiritual needs, fostering a sense of peace and dignity in their final days.
In palliative care, caregivers often have a more hands-on role in managing symptoms. This includes administering medications, attending doctor’s appointments, and facilitating open communication between healthcare providers. Caregivers may also need to monitor their loved one’s physical and emotional changes, ensuring the palliative care team adjusts the treatment plan as necessary. Coordinating with the care team ensures that the patient’s symptoms are controlled and their quality of life is maximized.
Self Care for Caregivers
Self-care is essential for caregivers in hospice and palliative care settings. To manage their own emotional well-being, caregivers should seek out support groups, therapy, or counseling. Respite care, where others provide temporary relief, can give caregivers time to rest and recharge. We can help you find free yoga classes, find time to enjoy hobbies or activities that nourish your well-being and seek guidance so you’re able to learn how to cope with the stress of caregiving for a loved one. Careers can continue to provide compassionate and effective support for their loved ones by taking care of themselves.

Myths and Misunderstandings
There are common myths surrounding hospice care, with many believing it means “giving up” or hastening death. In reality, hospice focuses on providing comfort, dignity, and quality of life during a patient’s final months. It doesn’t accelerate death but ensures patients spend their remaining time in peace, managing pain and emotional distress holistically through a compassionate team of professionals.
Similarly, a common misconception about palliative care is that it’s only for end-of-life situations. In truth, palliative care can be integrated at any stage of a serious illness alongside curative treatments. Its purpose is to manage symptoms and improve the quality of life for patients, whether they are undergoing treatments or not.
Caregivers may hesitate to consider hospice or palliative care due to emotional barriers or misconceptions. To overcome these hesitations, caregivers should focus on open communication with healthcare providers and educate themselves about the benefits of both care types. Seeking guidance from professionals or support groups can help caregivers make informed, compassionate decisions.
Please know that Wings of Hope is only a phone call away for a complimentary evaluation for your loved one. We can be reached 24 hours a day at (602) 971-0304.
Choosing the Right Care for Your Loved One
Hospice and palliative care aim to improve a patient’s quality of life, but they differ in timing and treatment focus. Hospice care is for those nearing the end of life, where curative treatments are no longer pursued, focusing solely on comfort and dignity. Palliative care, on the other hand, can be provided at any stage of a serious illness alongside treatments aimed at recovery, emphasizing managing symptoms and enhancing overall well-being.
Caregivers should feel reassured that both hospice and palliative care prioritize the comfort, dignity, and emotional needs of their loved ones. Each option offers holistic support for the patient and the family.
Caregivers need to consult with healthcare providers to understand which type of care is most appropriate based on their loved one’s specific needs and condition. Open communication ensures that the best decision is made for the patient’s well-being.